Clinical trials are a type of clinical study that thoroughly examine the safety and efficacy of interventions (new drugs, existing drugs, drug combinations, devices, treatment methods, etc.) on humans. The backbone of the clinical trial process is progressing stages called phases from 0 or 1 up to 5. Through these, the goal is to verify the safety and efficacy of the new treatment.
There is no exact time frame for a clinical trial. Some can be urgently expedited, but others can take up to 10–15 years from start to approval. Each phase has a different purpose, period, participant number, and protocols.
And each marks another step forward. Knowing the contents of the specific phase will guide your understanding of a trial, so that’s what this article covers.
What you’ll learn in this post
• What the aims of clinical trials are and how they are achieved.
• What “phases” are in clinical trials.
• What each phase, from 0 or I (1) to IV (4) aims to achieve.
• How you can be matched with a publication expert to help with all stages of your trial.
Why do clinical trials have phases?
Clinical trials must be divided into different phases, considering the differences between the aims and regulations of each phase. At the beginning of the research, the main goal is to find the dosage, check safety, reveal potential toxicity, and to discover side effects. Later stages investigate whether the new drug or treatment is more beneficial than an existing one.
The phases are closely connected, and the potential new drug or treatment must reach the target of every single stage to move forward. Failure in any phase means the drug cannot be approved for human use and, thus, cannot be approved for commercialization.
The number of participants increases in each phase until approval. At the early stage, the intervention is tested on a small population. Later, the number of patients can reach up into the thousands for diverse, robust, reliable data.
Phases 0 through IV
Before clinical research can start, the trial must be approved by the appropriate authority in the country developing the drug. This will let the investigational new drug (IND) be tested in humans.
Previously, preclinical studies have been performed, including cell cultures and mouse models.
Phases I to III are the three main stages before the treatment can be approved. Phases 0 and IV are also used to get a complete picture of the new drug or treatment method.
Phase 0: New intervention, small dose, small group
The U.S. Food and Drug Administration (FDA) introduced phase 0 (what is essentially early phase I) studies in 2006, though they’re not mandatory.
This phase involves a small group of people, usually around 10–40 volunteers. The dosage is far below the therapeutic dose. This is called micro-dosing, and it makes it very unlikely that the dose will cause any serious side effects.
The main targets here are finding out:
- What happens to the drug in the body?
- How does the body respond to the drug?
- Does the drug reach the target cells?
- How long does the drug stay in the body?
A phase 0 trial can provide an early look into humans before the pharmaceutical company invests in a full-scale phase I program. But it might be time-consuming. When speed is important, this may be the main factor for skipping phase 0.
Phase 0 trial example
One example is this phase 0 study on an Alzheimer’s drug. The researchers examined the brain uptake, retention, and safety on 36 participants. Through this, they acquired preliminary information about the drug.
Phase I (Phase 1): Testing the dose and side effects
Like phase 0, phase I still examines healthy volunteers, but the number of participants is usually around 20–100.
This phase’s main purpose is to ensure the treatment’s general safety, find the proper dosage, and discover possible serious adverse events. Adverse events can be any toxic or undesirable effect that may cause danger to health, such as permanent damage, disability, birth disorders, or heart attack. This phase usually takes a few months. Phase 1 trials carry the most potential risks for the participants.
At the end of phase I, the test results are collected, analyzed, and submitted to the authorities for permission to move forward to phase II. If the treatment was associated with one or more serious adverse events, the FDA (in the case of the US) may not give approval to proceed with the trial. However, if the results of phase I meet the primary outcomes, the study can move to phase II.
Phase I trial example
This study shows an always current topic: seasonal influenza. In the trial, a potential vaccine adjuvant was evaluated for safety and immune reactions in healthy adult volunteers.
The study had 36 participants: 24 received the vaccine with the investigated adjuvant, and the other 12 received the standard seasonal influenza vaccine. The investigated substance was found to be well-tolerated, safe, and a novel adjuvant for human influenza vaccines.
Phase II (Phase 2): Efficacy in a larger group
In phase II, researchers examine a larger group of people, up to several hundred, who have the disease the drug is being developed to treat. Phase II trials aim to find the best dose of the drug regarding its effectiveness and safety, and to discover any other possible side effects.
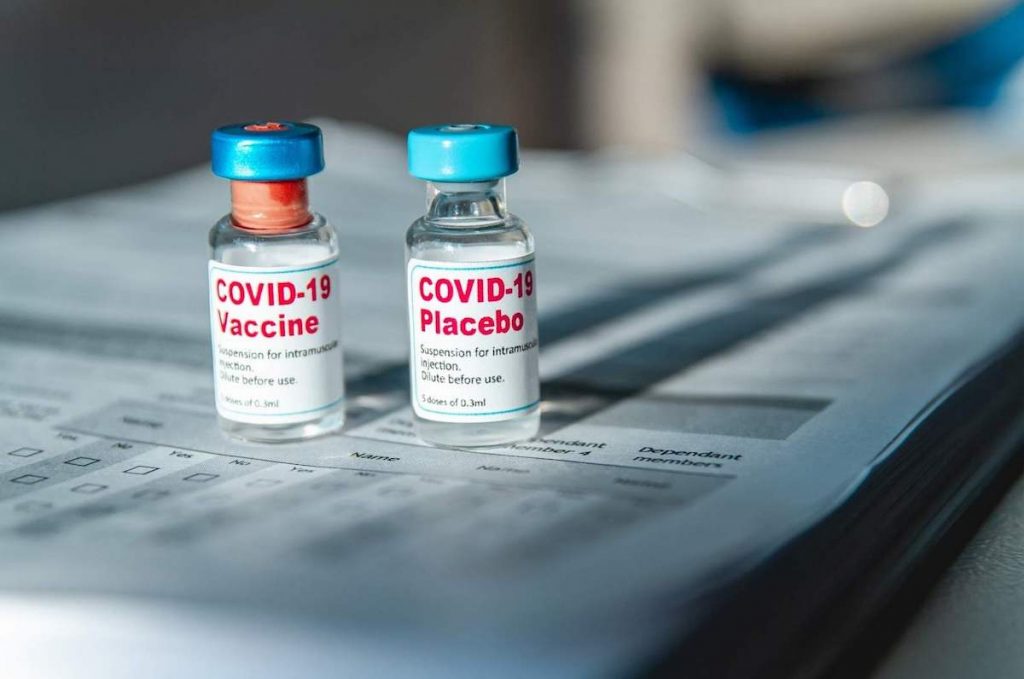
The participants are usually assigned into different treatment groups, where each group can receive a different dose or administration. Normally, there’s also a control group that receives the current standard treatment or a placebo. For ethical reasons, a placebo is never used alone if there’s an available therapy that works. The usual length of this phase is from 6 months to 2 years.
Phase II trial example
This study shows a phase II clinical trial about inoperable HPV (human papillomavirus)-related cancer. It aimed to determine whether the efficacy of nivolumab, an anti-checkpoint antibody, is amplified through treatment with the HPV-16 vaccine.
Of 23 patients, the overall response was 33%, and the median overall survival was 17.5 months, which is considered promising. However, toxicity occurred in two patients, requiring discontinuation of nivolumab therapy.
Phase III (Phase 3): Extensive safety and applicability
Phase III clinical trial involves a larger group of people, up to a few thousand.
This stage primarily focuses on assessing whether the treatment is safe and effective for a wide variety of patients. This phase also involves dividing participants into two or more groups: treatment and control groups. The control group receives the current standard treatment or a placebo.
Phase III is the last stage before the clinical trial results are submitted to the regulatory authorities for approval.
These studies are often performed in different cities and in different countries around the world and at the same time to ensure the greatest possible variety of patients. The phase typically lasts around 1–4 years.
Phase III trial example
During the coronavirus pandemic, large, high-quality clinical trials were required to develop treatment. And they needed to be expedited.
In this study, favipiravir was tested in a phase III trial to assess the efficacy and safety of the drug in adults with mild to moderate symptoms. Patients were divided into two groups. One group received favipiravir and supportive therapy, while the other received only supportive treatment.
Adverse events were observed in 36% of favipiravir-receiving patients and 8% of control patients. As a result, significant improvement in time to clinical cure suggests favipiravir may be beneficial in mild-to-moderate COVID-19.
Phase IV (Phase 4): Post-approval, long-term safety
Phase IV is quite different from the previous steps, as it investigates the drug’s life after approval.
It’s also known as post-marketing surveillance or a drug monitoring trial. The aims are to assure long-term safety and effectiveness, investigate interactions with other drugs, and uncover any rare side effects. This phase makes it possible to detect any rare or long-term adverse effects over a larger group of people and a longer period than what’s found in phases I to III.
If this phase reveals serious concerns about the treatment, the treatment may be withdrawn from the market or restricted to certain uses.
Phase IV trial example
One example, an anti-inflammatory substance, rofecoxib showed serious cardiac side effects during a phase IV and was withdrawn from the market. Rofecoxib was a modern painkiller that promised a breakthrough for joint pain.
Unlike other NSAIDs, it caused negligible gastrointestinal side effects. It was introduced to the market in 1999 and then withdrawn in 2004 because taking the drug caused serious cardiovascular risk.
Get assistance with your clinical studies
Whether you’re planning your study or writing up the results, Edanz’s researcher services can match you with an expert. And our service can help you and your colleagues achieve impactful research at a global standard. Explore Edanz services here. Get an expert scientific review of your study. Get in touch to see how we can help you.